How AI Is Transforming Skin Cancer Detection: From Dermoscopy to Teledermatology
Skin cancer remains one of the most common forms of cancer worldwide, with melanoma and non-melanoma types continuing to rise in incidence. The good news is that early detection significantly increases the chances of successful treatment – and advances in artificial intelligence (AI) are making that process faster, more accessible, and in some cases, more accurate than ever before.
In our clinic, we continue to rely on experience-led assessments and professional judgement when diagnosing skin cancers. However, we’re also closely watching the way AI is reshaping the landscape of dermatological care. From enhanced dermoscopic analysis to algorithm-driven triage in teledermatology, AI is proving to be a valuable tool – not a replacement – in supporting clinical decision-making.
In this post, we’ll look at what skin cancer is, how it’s traditionally detected, and how emerging AI tools are changing the way we assess, diagnose and manage suspicious skin lesions.

Understanding Skin Cancer: Melanoma vs Non-Melanoma
Skin cancer develops when abnormal cells grow uncontrollably in the skin. While there are multiple subtypes, we primarily focus on two categories in clinical practice:
Melanoma
Melanoma arises from melanocytes – the pigment-producing cells in the skin. It’s the most serious form of skin cancer and has a higher likelihood of spreading (metastasising) to other parts of the body if not caught early. Melanoma may appear as a new mole or a change in an existing one, often showing irregular shape, colour variation, or evolving symptoms such as itching or bleeding.
Non-Melanoma Skin Cancers (NMSC)
This category includes:
- Basal cell carcinoma (BCC): The most common but least likely to spread. It often appears as a pearly bump or sore that doesn’t heal.
- Squamous cell carcinoma (SCC): More likely to grow deeper into the skin, often presenting as a scaly, red patch or wart-like lesion.
While NMSCs are usually less dangerous than melanoma, all types of skin cancer benefit from early recognition and treatment.
For more on symptoms and screening, visit our Mole Screening and Skin Cancer Detection Service.
Traditional Detection Methods
For decades, the gold standard for skin cancer detection has been a face-to-face dermatological assessment, sometimes followed by dermoscopy and, if necessary, a biopsy.
Dermoscopy
Dermoscopy (or dermatoscopy) involves using a handheld device called a dermatoscope to magnify and illuminate the skin, allowing us to examine pigmented lesions in much greater detail. It reveals sub-surface structures, patterns and colours not visible to the naked eye.
A trained dermatologist will interpret these visual clues based on years of experience, guided by pattern recognition and diagnostic algorithms such as the ABCDE rule or the 7-point checklist.
Biopsy and Histopathology
If a lesion looks suspicious, a skin biopsy is taken and analysed by a pathologist under a microscope. This confirms whether the lesion is benign, pre-cancerous, or cancerous – and if so, what type.
The Role of Artificial Intelligence in Skin Cancer Detection
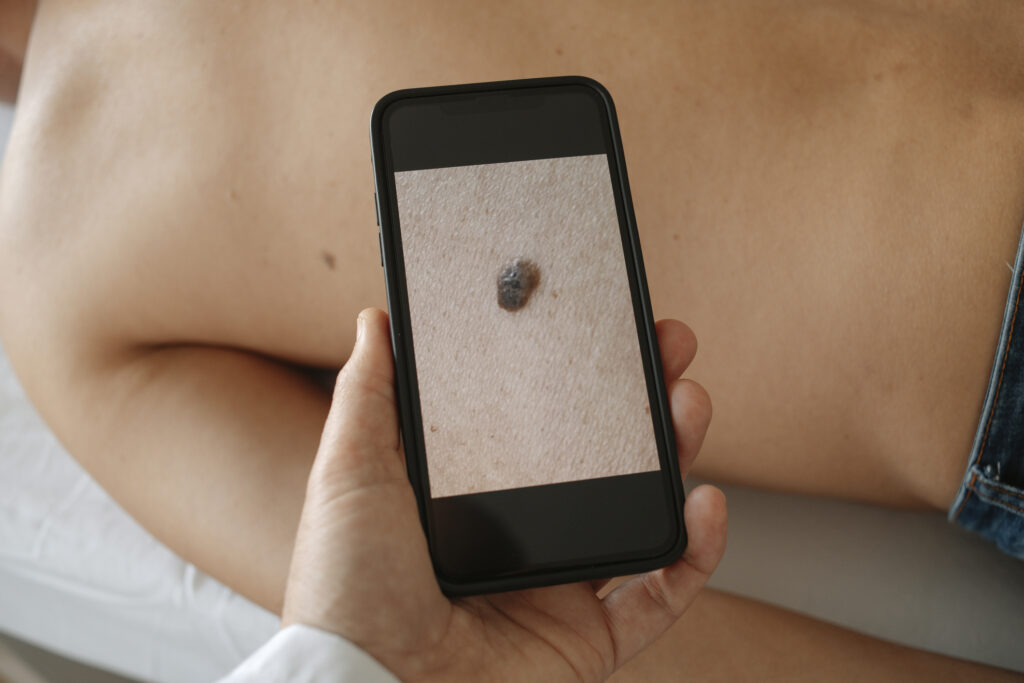
In recent years, AI-powered diagnostic tools have shown promise in supporting early detection, particularly in assessing dermoscopic images of skin lesions.
AI models – particularly those built on deep learning neural networks – are trained on thousands (or even millions) of labelled skin images. By learning to recognise patterns associated with different skin conditions, these systems can eventually identify suspicious lesions and differentiate between benign and malignant growths.
A landmark 2020 study published in Nature found that a deep learning model could outperform board-certified dermatologists in classifying skin lesions based on images. Other studies, including one led by the University of Heidelberg, demonstrated that AI could achieve diagnostic accuracy comparable to or better than dermatologists, particularly in identifying melanoma.
Key advancements include:
- Image-based diagnosis: AI tools can analyse dermoscopic and clinical images, flagging lesions for further review by a human clinician.
- Automated triage: In teledermatology platforms, AI can prioritise high-risk cases for faster follow-up.
- Decision support: AI can offer probability scores or risk levels, supporting dermatologists in decision-making.

AI in Practice: Benefits and Limitations
While the technology is impressive, AI doesn’t replace the need for clinical judgement. From our perspective, the most valuable use of AI is as an assistive tool, helping dermatologists assess lesions more efficiently, reduce diagnostic variation, and triage patients more effectively in remote consultations.
Benefits:
- Faster assessments, particularly in high-volume clinics
- Improved access to care in underserved or rural areas
- Consistent risk scoring across large patient populations
- Reduction in unnecessary biopsies of benign lesions
Limitations:
- AI is only as good as the dataset it’s trained on – and some populations (e.g. darker skin tones) are underrepresented in training sets
- It cannot assess patient history, lesion behaviour over time, or systemic symptoms
- Visual image quality and lighting conditions can affect diagnostic accuracy
- Over-reliance may risk missing complex or rare presentations
As outlined in reviews from the Cleveland Clinic and Mayo Clinic, human interpretation remains essential – especially when managing ambiguous cases or conducting full-body skin checks.
The Future: Integrating AI Into Dermatology Services
Here at The Devonshire Clinic, we believe the future lies in blending medical expertise with technology – not replacing one with the other. AI may soon play a larger role in:
- Teledermatology triage for GP referrals
- In-clinic dermoscopic analysis to support second opinions
- Risk prediction models for patients with multiple moles or family history of skin cancer
- Patient self-monitoring apps, empowering individuals to track moles and skin changes over time
However, no AI tool can yet replicate the full scope of a dermatologist’s clinical judgement, nor provide the reassurance, experience and nuanced care that patients need during skin cancer diagnosis and treatment.
That’s why we continue to offer in-person mole screening and consultant-led dermatology services, supported where appropriate by the latest diagnostic technology.
Frequently Asked Questions
Can AI detect skin cancer on its own?
AI can assist in identifying suspicious lesions, especially from dermoscopic images, but it should always be used alongside clinical assessment. It’s not a substitute for a dermatologist.
Is AI used in UK dermatology clinics?
Yes, several NHS and private providers are piloting AI tools for triage and image analysis, especially in teledermatology services. Adoption is increasing, but always with a clinician’s oversight.
Is AI more accurate than a dermatologist?
Some studies show that AI models can match or exceed dermatologist-level accuracy in image classification. However, diagnosis involves more than just an image – so human expertise remains essential.
Can I use an app to check my moles?
There are AI-based mole-checking apps available, but they vary in quality and reliability. We recommend using them cautiously and following up with a professional mole screening if you have concerns.
Expert Skin Cancer Screening – Powered by People, Informed by Tech
AI may be reshaping the way we detect and manage skin cancer, but at its heart, good dermatological care still depends on trained, experienced professionals. Whether you’ve noticed a changing mole, need a second opinion, or simply want reassurance, we offer detailed assessments tailored to your needs.
To book a skin check or learn more about our Mole Screening Service, visit our website or contact our team today.