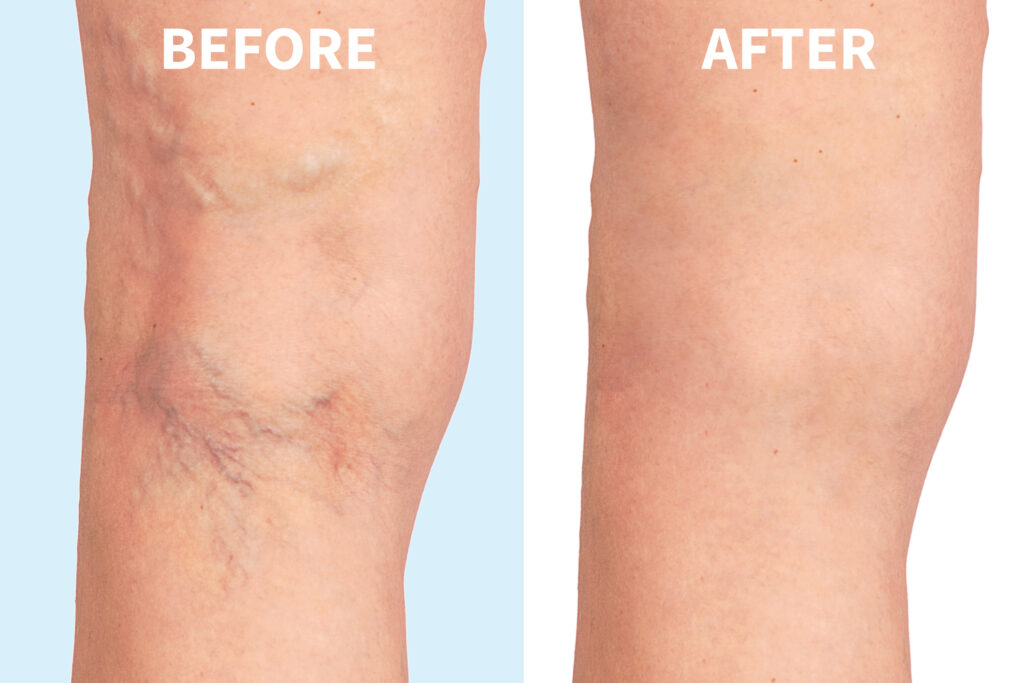
Thread veins—also known as spider veins or telangiectasia—are a common cosmetic concern that affects many people, especially as they age. These tiny, visible blood vessels often appear just beneath the skin’s surface and can cause self-consciousness or discomfort, even though they are typically harmless. At The Devonshire Clinic, we offer expert insight and treatment options […]
Everything About Thread Veins: Causes, Treatments, and What to Expect